Flu Season Explained: A Guide to Symptoms and Prevention Tips
Outline:
– Section 1: Why Flu Season Matters—Scope, who is affected, and why it recurs
– Section 2: When and Why It Peaks—Climate, behavior, and geography
– Section 3: Recognizing Symptoms—How flu differs from other infections
– Section 4: Prevention That Works—Vaccines, hygiene, and indoor air
– Section 5: Care and Recovery—Treatment options and a community-focused conclusion
Why Flu Season Matters: A Quick Orientation
Every year, flu season settles in like a familiar storm front: expected, yet still disruptive. The influenza viruses that drive it change subtly over time, which means communities face a recurring challenge rather than a one-off event. In a typical year, millions fall ill worldwide, and hundreds of thousands experience severe disease, with outcomes that strain clinics, families, and workplaces. Those numbers swing widely depending on how well circulating viruses align with immune protection in the population, how early prevention steps roll out, and how people behave as temperatures drop.
Why does it matter so much? Because influenza is more than a nuisance. Rapid fever, aches, and exhaustion can sideline a healthy adult for days and complicate chronic conditions. The impact ripples outward: caregivers miss work, schools see absences, and small businesses navigate unpredictable staffing. When multiple community layers are hit at once, even routine scheduling can feel like juggling in a windstorm. Older adults, people with chronic heart or lung conditions, those with weakened immune systems, and those who are pregnant face higher risks of complications. For them, a “bad cold” can become a serious lower respiratory illness or trigger a cascade of health setbacks.
Flu season also informs public planning. Pharmacies prepare for demand swings, clinics adjust staffing, and schools refresh absence policies. Households stock up on tissues and soups, while offices revisit sick-leave norms that keep a single cough from turning into a department-wide wave. These patterns are not only predictable; they are actionable. Clear information helps people choose protective steps at the right time—from getting an annual shot to improving indoor air, from washing hands regularly to staying home when feverish. Think of flu season as the community’s annual stress test: preparation softens the blow, and small daily decisions add up to meaningful protection.
When and Why It Peaks: Timing, Climate, and Behavior
Flu season does not strike every place at once, and its timing reveals how biology and behavior intertwine. In many northern regions, activity usually rises in late fall, peaks between December and February, and tapers by early spring. In southern regions, cooler months tend to shoulder the burden, often from May through September. Near the equator, influenza can circulate year-round with pulses that follow rainy seasons or school calendars. This geographic rhythm reflects several overlapping drivers rather than a single cause.
Climate plays a role. Laboratory and field studies suggest that lower absolute humidity and cooler temperatures help influenza viruses persist and travel farther in airborne particles. Dry indoor air, common in heated buildings, can irritate nasal passages and potentially make it easier for viruses to take hold. Winter sun is lower, people spend more hours indoors, windows close, and fresh air exchange slows. Meanwhile, social patterns shift: holidays bring travel and gatherings, schools and offices concentrate people in shared spaces, and public transit grows busier. Each factor is small on its own, but together they give the virus more opportunities to move.
Behavior amplifies or dampens these seasonal forces. A classroom with windows cracked for a few minutes each hour dilutes aerosols more effectively than a sealed room. A household that keeps a simple “stay home when feverish” rule cuts transmission chains. Communities that begin vaccination campaigns before local activity ascends often see fewer severe outcomes once the wave arrives. Timing matters because protective measures are not instant; they work best when layered and started early.
Consider three practical signals:
– Watch local health dashboards or school absenteeism as early clues of rising activity.
– Track indoor crowding: buses, elevators, and break rooms become higher-risk as ventilation drops.
– Note weather and holiday calendars: the combination of cold snaps and gatherings often precedes upticks.
Ultimately, flu season’s peak is the outcome of physics, physiology, and daily routines. By adjusting the controllable parts—airflow, timing of vaccination, and practical habits—communities can bend the curve, even if they cannot erase the season altogether.
Recognizing Symptoms and Telling Flu from Other Illnesses
Influenza often announces itself with a sudden jolt. One day you feel normal; the next, fever and deep fatigue arrive like a flipped switch. Common symptoms include:
– High fever or chills, often early in the illness
– Dry cough that can become persistent
– Sore throat and runny or stuffy nose
– Headache, body aches, and notable fatigue
– Occasionally nausea or diarrhea, more often in children
How does flu differ from a routine cold? Colds typically creep in: a scratchy throat, a slow-onset drip, and milder aches. Fever is less common and usually lower if present. Flu hits faster, hurts more, and can leave you craving sleep even after a full night’s rest. That said, respiratory illnesses overlap. Other viruses can cause fever and cough, and some can mimic influenza closely. When symptoms are severe, when you are part of a higher-risk group, or when community influenza activity is high, testing can guide care and timing of prescription treatments.
What about differentiating from other respiratory infections making the rounds? While specific symptom patterns can hint at the culprit, no single sign is definitive. Loss of taste or smell is less typical for influenza than for some other viruses, though it can occur. Shortness of breath that worsens, chest discomfort, or bluish lips or face are warning signs that warrant urgent evaluation regardless of the cause. Dehydration, confusion, or persistent high fever are additional red flags.
Practical tips for self-monitoring:
– Track the first day you felt truly unwell; a clear start helps assess timing for treatments.
– Note maximum temperature and how often you need fever reducers.
– Watch your breathing during light activity; rising effort or wheezing should prompt a call to a clinician.
Remember, general guidance is helpful, but it does not replace personalized medical advice. If you are pregnant, caring for an infant, managing chronic conditions, or supporting an older adult, early contact with a healthcare professional can streamline decisions and reduce the chance of complications. When in doubt, ask—clarity is part of good care.
Prevention That Works: Vaccination, Hygiene, and Indoor Air
Protecting yourself during flu season is not about a single heroic step; it is about layering simple actions that nudge risk downward. Start with vaccination. Seasonal shots are updated to match anticipated strains and are designed to reduce the chance of illness and, importantly, to lower the risk of severe outcomes like hospitalization. Effectiveness varies by year and by age group, but even in seasons with modest protection, vaccinated people often experience milder disease if infected. Because it takes about two weeks for immunity to build, earlier is better—ideally before local activity surges.
Next, elevate everyday habits. Hands are vehicles for germs, especially after touching shared surfaces and before eating. Wash with soap and water for about 20 seconds, or use an alcohol-based sanitizer when sinks are not handy. Cover coughs and sneezes with a tissue or your elbow, and dispose of tissues promptly. Keep a small care kit at home and work with tissues, sanitizer, and a spare mask for days when a sore throat appears at midday. Rest, balanced nutrition, and adequate sleep support the immune system’s baseline performance; small, consistent choices win here.
Indoor air deserves special attention. Many infections occur in shared indoor spaces where the virus can linger in aerosols. Improving ventilation dilutes those particles. Simple measures help:
– Open windows for a few minutes each hour when weather allows.
– Use portable air cleaners with high-efficiency filters sized to the room.
– Maintain HVAC filters and check their ratings during seasonal tune-ups.
– Avoid overcrowding small rooms; stagger meetings or use larger spaces when feasible.
Masks can be useful in crowded, poorly ventilated settings, especially when local activity is high or if you are protecting someone with higher risk. If you choose to wear one, ensure a snug fit over the nose and mouth. Community-minded policies also matter: straightforward sick-leave practices, flexible deadlines during peak weeks, and communication about local trends all reduce spread.
Think of prevention as a patchwork quilt—each square adds warmth, but together they cover more of the chill. Vaccination, hygiene, and cleaner air are the core pieces. Add common-sense choices like staying home with fever, and you have a practical, sustainable plan that respects daily life while trimming risk.
If You Get Sick: Care, Antivirals, and a Community-Minded Conclusion
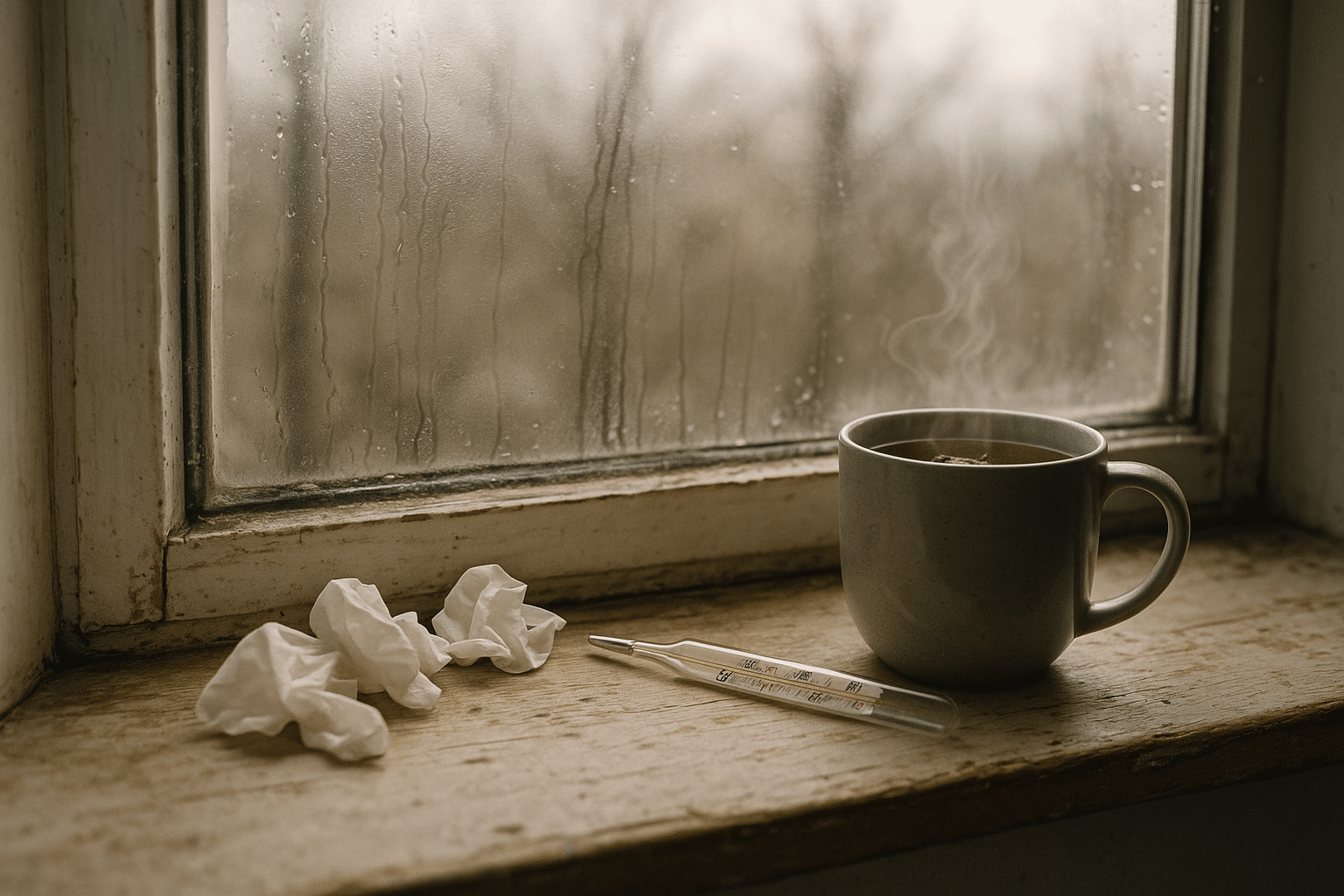
Even with strong prevention, influenza can break through. When it does, early, simple steps make recovery smoother. Rest is your ally; your body spends significant energy fighting infection. Drink fluids steadily—water, broths, and warm teas ease sore throats and help prevent dehydration. Gargling warm salt water can soothe discomfort, and a humidifier can moisten dry air if cough worsens at night. Over-the-counter medicines may reduce fever or ease aches; follow label guidance and seek advice if you manage chronic conditions or take multiple medications.
Antiviral prescriptions can be considered, especially for those at higher risk or those with severe symptoms. They work best when started within the first 48 hours of illness and can shorten the duration of symptoms and reduce the likelihood of complications. Not everyone needs them, so a quick call to a clinician—ideally with your symptom timeline—helps determine fit. Avoid giving aspirin to children and teenagers with viral illnesses due to the risk of rare but serious complications. Honey can soothe cough in children older than one year, but should not be given to infants.
When to seek medical attention:
– Breathing that becomes difficult, fast, or painful
– Chest pain, persistent dizziness, or new confusion
– Dehydration signs: infrequent urination, dry mouth, or extreme fatigue
– Fever that returns or persists beyond several days
– Worsening symptoms in people who are pregnant, older adults, or those with chronic conditions
Isolation guidance is practical and considerate. Stay home until at least 24 hours after your fever resolves without fever-reducing medicine. Communicate with your employer, school, or teammates early so plans can shift without drama. Keep shared spaces tidy: frequently touched surfaces like doorknobs and remotes benefit from routine cleaning during illness. A small wastebasket beside the bed for tissues, a dedicated water bottle, and a reminder to air out the room a few times a day create a recovery-friendly setup.
Conclusion for readers navigating busy lives: flu season is an annual visitor, but it need not dictate your calendar. A timely shot, a habit of washing hands, better indoor air, and the wisdom to rest when feverish form a workable toolkit for families, students, and professionals alike. If illness strikes, early care and thoughtful isolation protect both you and the people around you. With preparation and calm, you can move through the season with steadier footing—and return to your routines with energy in reserve.